Is Nipple Vasospasm dangerous? Understand the Symptoms and find effective treatments!

Nipple vasospasm, while not typically dangerous, can be an incredibly uncomfortable and distressing condition for breastfeeding mothers. It occurs when blood vessels in the nipples constrict, leading to symptoms such as severe pain, discoloration, and sensitivity. Understanding the signs and finding effective treatments is crucial for relieving discomfort and maintaining successful breastfeeding. In this blog, we will delve into the symptoms of nipple vasospasm and explore various treatment options to help mothers navigate this challenging issue, promoting a more comfortable and enjoyable breastfeeding experience.

In this blog, we will explore what nipple vasospasm is, its causes, symptoms, and potential management strategies.
What is Nipple Vasospasm?
Nipple vasospasm, also known as Raynaud’s phenomenon of the nipple, is a condition characterized by the constriction or narrowing of blood vessels in the nipple. This constriction restricts blood flow, leading to symptoms such as pain, discoloration, and sensitivity in the nipple area.
Is nipple vasospasm dangerous?
Nipple vasospasm itself is not considered dangerous. It is a benign condition that, while uncomfortable and sometimes painful, does not pose significant health risks. However, it can impact a woman’s breastfeeding experience and overall comfort during pregnancy.
It is important to note that nipple vasospasm can be a symptom of an underlying issue, such as Raynaud’s disease, which affects blood vessels in various parts of the body. In such cases, it is advisable to consult with a healthcare provider for further evaluation and appropriate management.
While nipple vasospasm is generally not dangerous, it is crucial to seek medical advice if you experience severe or persistent symptoms, as this could indicate other potential causes or complications. Your healthcare provider can assess your specific situation, provide a proper diagnosis, and offer guidance on management strategies to alleviate symptoms and ensure your well-being
What causes Nipple Vasospasm During Pregnancy?
The nipple vasospasm caused during pregnancy is not fully understood. However, several factors are believed to contribute to its development:
- Hormonal changes: Pregnancy causes significant hormonal fluctuations, including increased levels of estrogen and progesterone. These hormonal changes can affect blood vessels, making them more prone to vasospasm.
- Cold exposure: Exposing the breasts to cold temperatures or sudden temperature changes can trigger vasospasm in susceptible individuals.
- Breastfeeding issues: Nipple vasospasm can sometimes be associated with breastfeeding difficulties, such as improper latch, poor positioning, or ineffective milk removal. These factors can lead to increased pressure and trauma on the nipple, contributing to vasospasm.
How long does nipple vasospasm last?
The duration of nipple vasospasm can vary from person to person and depends on several factors, including the underlying cause, how well the condition is managed, and individual healing abilities. In some cases, nipple vasospasm may resolve relatively quickly with appropriate management, while in others, it may persist for a longer period.
With proper care and management, many cases of nipple vasospasm improve within a few days to a couple of weeks. Keeping the nipples warm and protected, ensuring a correct latch and positioning during breastfeeding, and avoiding exposure to cold temperatures are essential aspects of managing nipple vasospasm.
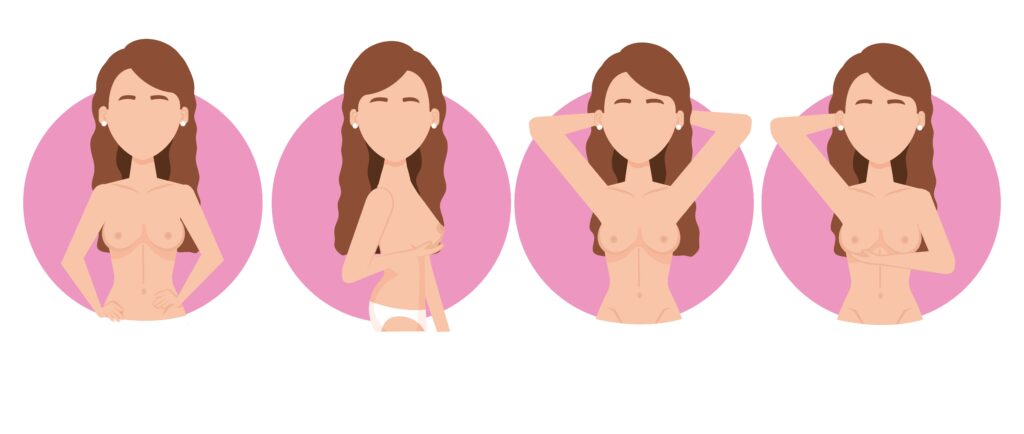
What are the symptoms of Nipple Vasospasm?
Nipple vasospasm typically presents with the following signs and symptoms:
- Nipple pain: A sharp, burning pain in the nipple, often described as throbbing or stinging, is a common symptom of vasospasm.
- Nipple discoloration: The affected nipple may appear pale, bluish, or mottled due to reduced blood flow.
- Nipple sensitivity: Nipples may become extremely sensitive to touch, cold temperatures, or even slight pressure.
- Pain triggered by cold: Exposure to cold air, cold water, or even a cold room can trigger or worsen the pain associated with nipple vasospasm.
Nipple vasospasm vs thrush
Nipple vasospasm and thrush are two different conditions that can affect breastfeeding women. Both can cause discomfort and pain during breastfeeding, but they have distinct causes and treatments. Here’s a brief explanation of each:
- Nipple Vasospasm: Nipple vasospasm, also known as Raynaud’s phenomenon of the nipple, is a condition characterized by the constriction of blood vessels in the nipple area, leading to reduced blood flow and subsequent color changes in the nipple. It often occurs in response to exposure to cold temperatures or due to excessive pressure on the nipple during breastfeeding. Symptoms of nipple vasospasm may include sudden, sharp pain or burning sensation in the nipple after feeding, and the nipple may appear blanched, white, or blue.
Treatment for nipple vasospasm involves keeping the nipples warm and protected, especially during and after breastfeeding. This can be done by wearing warm clothing, using heating pads or warm compresses, and avoiding exposure to cold temperatures. It’s also essential to ensure proper latch and positioning during breastfeeding to minimize nipple trauma.
- Thrush (Breast and Nipple Candidiasis): Thrush is a fungal infection caused by an overgrowth of the Candida albicans yeast. It can occur in the baby’s mouth (oral thrush) and can be transmitted to the mother’s nipples during breastfeeding, leading to nipple and breast pain. Symptoms of thrush in breastfeeding mothers may include nipple pain, itching, burning, or shooting sensations, often lasting throughout or after the feeding. The nipples may appear red, shiny, or flaky, and there might be shooting pains deep within the breast.
To treat thrush, both the mother and the baby need to be treated simultaneously, even if the baby doesn’t show any obvious signs of oral thrush. The treatment usually involves antifungal medications, such as topical creams for the nipples and oral suspension for the baby’s mouth. Additionally, maintaining proper nipple hygiene and allowing the nipples to air dry after feeding can help prevent the spread of the infection.
If a breastfeeding mother is experiencing nipple pain or discomfort, it’s essential to seek help from a lactation consultant, a healthcare provider, or a breastfeeding support group. They can help determine the underlying cause of the issue and provide appropriate guidance and treatment.
How can I manage the Nipple vasospasm?
If you suspect you are experiencing nipple vasospasm during pregnancy, it is essential to consult with your healthcare provider. They can assess your symptoms, rule out other potential causes, and provide appropriate guidance. Here are some management strategies that may be recommended:
- Warmth and insulation: Keeping the nipples warm is crucial in managing vasospasm. Wearing well-fitting, warm clothing, and using warm compresses before and after breastfeeding can help alleviate symptoms.
- Correct breastfeeding techniques: Ensuring a proper latch and positioning during breastfeeding can minimize nipple trauma and reduce the risk of vasospasm. Seeking assistance from a lactation consultant or a breastfeeding specialist can be beneficial.
- Avoidance of triggers: Minimizing exposure to cold temperatures or sudden temperature changes is important. Layering clothing, using nipple shields, or applying a protective ointment can offer additional insulation.
- Medication: In severe cases, your healthcare provider may prescribe medications, such as calcium channel blockers or vasodilators, to relax the blood vessels and alleviate symptoms.
Conclusion
Nipple vasospasm during pregnancy can be a distressing condition for expectant mothers. Understanding the causes, recognizing the symptoms, and implementing appropriate management strategies can significantly improve the comfort and breastfeeding experience. Remember to consult with your healthcare provider for an accurate diagnosis and personalized advice. With proper care and support, nipple vasospasm can be effectively managed, allowing you to enjoy the beautiful journey of pregnancy and breastfeeding.
References
- Buck ML, Amir LH, Cullinane M, Donath SM; CASTLE Study Team. Nipple pain, damage, and vasospasm in the first 8 weeks postpartum. Breastfeed Med. 2014 Mar;9(2):56-62. doi: 10.1089/bfm.2013.0106. Epub 2013 Dec 31. PMID: 24380583; PMCID: PMC3934541.
- Buck, Miranda & Amir, Lisa & Cullinane, Meabh & Team, Susan. (2013). Nipple Pain, Damage, and Vasospasm in the First 8 Weeks Postpartum. Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine. 9. 10.1089/bfm.2013.0106.
- Jesus Avila-Vega, Enrique Urrea-Mendoza, Christy Lee; Raynaud’s phenomenon of the nipple as a side-effect of labetalol: Case report and literature review, Case Reports in Women’s Health, Volume 23,2019,e00135, ISSN 2214-9112,https://doi.org/10.1016/j.crwh.2019.e00135
- Douglas P. Re-thinking lactation-related nipple pain and damage. Womens Health (Lond). 2022 Jan-Dec;18:17455057221087865. doi: 10.1177/17455057221087865. PMID: 35343816; PMCID: PMC8966064.
FAQs
- Can nipple vasospasm during pregnancy affect breastfeeding?
Yes, nipple vasospasm can affect breastfeeding. The pain and sensitivity associated with vasospasm may make breastfeeding uncomfortable or painful. It can also lead to difficulties with latch and milk transfer. Seeking support from a lactation consultant or breastfeeding specialist can help address these challenges and provide guidance on proper breastfeeding techniques.
2. How long does nipple vasospasm during pregnancy last?
The duration of nipple vasospasm during pregnancy can vary from woman to woman. Some may experience occasional episodes that resolve on their own, while others may have more persistent symptoms. With appropriate management strategies, such as keeping the nipples warm, practicing correct breastfeeding techniques, and avoiding triggers, the frequency and severity of vasospasm episodes can be reduced over time.
3. Does nipple vasospasm go away on its own??
No, but there are several self-care measures you can take to alleviate nipple vasospasm symptoms. Keeping the nipples warm by wearing warm clothing, using warm compresses, or applying a warm ointment can help improve blood flow. Proper breastfeeding techniques, including ensuring a good latch and positioning, can minimize nipple trauma and reduce the risk of vasospasm. Avoiding exposure to cold temperatures and sudden temperature changes is also important.
4. Is nipple vasospasm during pregnancy a cause for concern?
Nipple vasospasm during pregnancy is generally not a cause for major concern. It is considered a benign condition that can be managed effectively with appropriate strategies. However, if you are experiencing severe or persistent symptoms, it is recommended to consult with your healthcare provider to rule out any other underlying issues and ensure proper management.
Note: Remember, every individual’s experience with nipple vasospasm can be different, so it’s essential to consult with your healthcare provider for an accurate diagnosis and personalized advice based on your specific situation.















+ There are no comments
Add yours