Understanding Placenta Increta: Know what Medical Research Reveals!
Pregnancy can bring joy but also unexpected challenges. Placenta increta, a rare yet serious condition, deserves our attention. This article delves into the intricacies of placenta increta, its dangers for expectant mothers, symptoms, causes, treatments, and how it compares to placenta percreta. We’ll also explore the latest medical research on this condition and its implications for the future.

What is Placenta Increta ?
Placenta increta is a rare and serious pregnancy complication characterized by the abnormal attachment of the placenta to the uterine wall. In this condition, the placenta invades and penetrates too deeply into the uterine muscle, specifically the myometrium, instead of remaining within the uterine lining as it does in a normal pregnancy.
The depth of invasion in placenta increta can vary, and it increases the risk of complications during childbirth, particularly excessive bleeding, as the placenta cannot be easily separated from the uterine wall.
How dangerous is it for pregnant women?
Placenta increta is a highly dangerous condition for pregnant women due to the significant risks. The primary danger associated with placenta increta is the potential for severe and life-threatening hemorrhage (excessive bleeding). Here’s why it is considered perilous:
- Invasive Attachment: Placenta increta involves the placenta invading and penetrating deeply into the uterine wall, specifically the myometrium. This abnormal attachment makes it challenging to separate the placenta after delivery, increasing the risk of bleeding.
- Risk of Uncontrolled Hemorrhage: When attempts are made to remove the placenta, the abnormal attachment can lead to the tearing of blood vessels within the uterine wall. This can result in uncontrolled hemorrhage, which can be life-threatening for the mother.
- Emergency Situations: Placenta increta often necessitates emergency medical intervention, including emergency C-sections or, in severe cases, a hysterectomy (removal of the uterus) to control bleeding and prevent complications.
- Preterm Birth: Placenta increta can increase the risk of preterm birth, which carries its own set of health risks for both the baby and the mother.
- Blood Transfusions: Due to the risk of severe bleeding, preparations for blood transfusions are often made in advance to ensure an adequate blood supply is available if needed during surgery.
Given these dangers, early detection through prenatal care and imaging is crucial for managing placenta increta. Timely and expert medical care is essential to mitigate the risks and ensure the safety of both the mother and the baby. Pregnant women with placenta increta require close monitoring and a well-coordinated medical team to navigate the challenges this condition presents.
What are the symptoms of Placenta Increta?
Placenta increta may not always present noticeable symptoms before delivery, and it is often diagnosed through imaging studies or during childbirth. However, in some cases, women with placenta increta may experience the following symptoms:
- Abnormal Bleeding: Unusual vaginal bleeding, especially in the later stages of pregnancy or during the third trimester, can be a sign of placenta increta. This bleeding may be painless and may not resemble typical menstrual bleeding.
- Pelvic Pain: Some women with placenta increta may experience mild to severe pelvic pain or discomfort. This pain can be persistent or intermittent.
- Decreased Fetal Movements: Reduced fetal movements or changes in the baby’s activity patterns could be a sign of placenta increta. This is because the placental abnormalities can affect fetal oxygen and nutrient supply.
- Preterm Contractions: Placenta increta can sometimes cause premature contractions, leading to preterm labor.
- Palpable Mass: In rare cases, a healthcare provider may be able to feel a firm, irregular mass during a physical examination.
It’s important to note that these symptoms are not exclusive to placenta increta and can overlap with other pregnancy complications. If any of these signs or symptoms are experienced during pregnancy, it is crucial to seek immediate medical attention for a proper diagnosis and appropriate management.
What causes Placenta Increta?
Placenta increta primarily results from irregularities in placental development and attachment during pregnancy. While its precise cause is not always clear, several risk factors contribute to its occurrence.
Women with a history of uterine surgeries, like C-sections, are at higher risk due to potential scar tissue interfering with proper placental attachment. Advanced maternal age, multiple pregnancies (e.g., twins), placental abnormalities, uterine anomalies, and even in vitro fertilization (IVF) have also been linked to an increased likelihood of placenta increta.
Early detection through prenatal care and imaging is crucial, as it helps healthcare providers manage this condition effectively and minimize risks during pregnancy and childbirth
What are the treatments of Placenta Increta?
The exact cause of placenta increta is not well understood, but it is believed to result from abnormalities in the placental development and attachment process. Several factors and risk factors have been associated with an increased likelihood of developing placenta increta. These include:
- Previous Uterine Surgeries: Women who have undergone previous uterine surgeries, such as C-sections, myomectomies (fibroid removal), or dilation and curettage (D&C), are at a higher risk of developing placenta increta. Scar tissue and disruptions in the uterine lining can create an environment conducive to abnormal placental attachment.
- Advanced Maternal Age: Women over the age of 35 are more likely to develop placenta increta, although the reasons for this association are not entirely clear.
- Multiparity: Having multiple pregnancies or carrying more than one fetus (e.g., twins or triplets) can increase the risk of placenta increta.
- Placental Abnormalities: Certain placental abnormalities, such as a low-lying placenta (placenta previa) or an unusually large placenta, have been linked to an elevated risk of placenta increta.
- Uterine Abnormalities: Anomalies or irregularities in the shape or structure of the uterus can predispose a woman to placenta increta.
- In Vitro Fertilization (IVF): Some studies suggest a potential association between pregnancies conceived through IVF and an increased risk of placenta increta, though the overall risk remains relatively low.
It’s important to note that while these factors may increase the likelihood of developing placenta increta, the condition can still occur without any identifiable risk factors.
Which is worse placenta increta or Percreta?
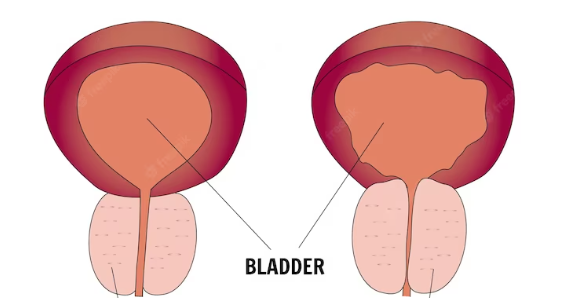
Placenta percreta is generally considered worse than placenta increta and Placenta accreta. Both conditions involve abnormal placental attachment to the uterine wall, but they differ in terms of the depth of invasion and potential complications:
Placenta Increta:
- In placenta increta, the placenta invades and penetrates deeply into the myometrium, which is the muscular layer of the uterus.
- The depth of invasion is limited to the myometrium and does not breach the uterine wall.
- While placenta increta is a serious condition that can lead to complications such as bleeding, it is usually less severe compared to placenta percreta.
Placenta Percreta:
- Placenta percreta is the most severe form of abnormal placental attachment.
- In this condition, the placenta not only invades the myometrium but also penetrates through the uterine wall, and it may even invade nearby organs like the bladder.
- Placenta percreta is associated with a higher risk of severe bleeding and complications during childbirth, making it more dangerous than placenta increta.
The severity of placenta percreta necessitates more complex and extensive medical interventions, including a higher likelihood of emergency hysterectomy (removal of the uterus) to control bleeding and prevent life-threatening complications. However, both conditions are serious and require careful management and coordination of medical care to ensure the best possible outcomes for the mother and the baby.
Conclusion
Placenta increta is a serious pregnancy complication characterised by abnormal placental attachment. Its dangers lie in the risk of severe bleeding and complications during childbirth. Early detection and vigilant prenatal care are essential for managing this condition effectively. Placenta increta must not be underestimated, but with proper medical attention and multidisciplinary care, there is hope for ensuring safer pregnancies and better outcomes for both mothers and their newborns.
Frequently Asked Questions:
- What distinguishes placenta increta from placenta percreta?
Placenta increta involves the placenta invading the uterine muscle, while placenta percreta penetrates even deeper, potentially affecting nearby organs.
2. Can placenta increta be prevented?
While not always preventable, early detection through prenatal care is crucial for better management.
3. What are the long-term implications for mothers with placenta increta?
Long-term implications may include fertility challenges and the need for cautious planning in future pregnancies.

















+ There are no comments
Add yours